Increase of temperature through laser therapy (e.g. IR-A)
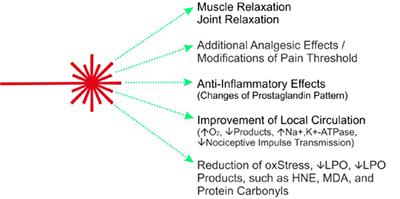
The main effect of laser heat therapy is muscle relaxation through thermoregulation. Thermoregulatory effects include increasing blood circulation to cool down when the body temperature rises above 37o Celsius. It leads to improved blood circulation and supply of oxygen and nutrients.
Metabolic waste products, carbon dioxide etc. are removed more quickly from the connective and muscle tissue. Anti-inflammatory effects as changes in the prostaglandin pattern have been described (Hardy et al., 1951; Moriyama et al., 2005; Pulichino et al., 2006; Rosseland et al., 2007).
Increased or normalised tissue pO2 and substrate supply increases or stabilises the activity of Na+-K+-ATPase. High Na+-K+-ATPase activity leads to reduced nociceptive impulse transmission (Moriyama et al., 2005).
Heat (IR irradiation) modifies the pain threshold (Khanapure et al., 2007). Further data indicate a reduction of oxidative stress.
Reduced lipid levels Peroxidation rate (LPO) and reduced plasma concentrations of toxic aldehydic LPO products such as malondialdehyde (MDA), 4-hydroxy-2,3-trans-nonenal (HNE) and protein carbonyls measured (Gruenberger, 2007).
MDA, HNE proteins and nucleic acids can be modified. Reduction of Na+-K+-ATPase activity, an enzyme related to nociception by aldehydic LPO products, has been described (Siems et al., 1996; 2003).
Metabolic waste products, carbon dioxide etc. are removed more quickly from the connective and muscle tissue. Anti-inflammatory effects as changes in the prostaglandin pattern have been described (Hardy et al., 1951; Moriyama et al., 2005; Pulichino et al., 2006; Rosseland et al., 2007).
Increased or normalised tissue pO2 and substrate supply increases or stabilises the activity of Na+-K+-ATPase. High Na+-K+-ATPase activity leads to reduced nociceptive impulse transmission (Moriyama et al., 2005).
Heat (IR irradiation) modifies the pain threshold (Khanapure et al., 2007). Further data indicate a reduction of oxidative stress.
Reduced lipid levels Peroxidation rate (LPO) and reduced plasma concentrations of toxic aldehydic LPO products such as malondialdehyde (MDA), 4-hydroxy-2,3-trans-nonenal (HNE) and protein carbonyls measured (Gruenberger, 2007).
MDA, HNE proteins and nucleic acids can be modified. Reduction of Na+-K+-ATPase activity, an enzyme related to nociception by aldehydic LPO products, has been described (Siems et al., 1996; 2003).
Laser therapy class 3B and class 4
- Orthopedics
- Sports medicine
- Physiotherapy
- Therapy of large and small areas
Effect of cold laser therapy (LLLT) and high intensity laser therapy (HILT)
With the advanced technique, RJ-Laser specializes in low level, high intensity laser for physical therapy to provide muscle relaxation and reduce the pain effectively!
Laser therapy, photobiomodulation, can be performed locally, reflex, conventionally or "complementarily". The natural holistic healing method is in the foreground, therefore special functions and frequency programs are integrated in the RJ laser devices, e.g. for laser resonance therapy.The following points have an influence on the success of the therapy:
1. power (and power density, W/cm2)
2. correct amount of energy (Joules/cm2)
3. duration of therapy
4. frequency modulation, frequency information (Hz)
5. treatment location (local, reflective)
The right amount of energy (J/cm2) at the destination
Does the laser equipment provide sufficient amount of energy (generally 4-6 J/cm2) and does it reach the destination, is it superficial or deep, punctual or extensive? Do the photons or the required amount of energy reach the target location and in what time? Is the required therapy time acceptable for the patient or does the therapist have to choose another laser class to compensate for the losses due to higher power?
The laser beam is reflected, scattered, absorbed and transmitted depending on wavelength and tissue. Strong absorption and reflection takes place below 600 nm and above 950 nm, the tissue is overheated depending on the power.
Which laser power is the best?
The power of a "cold laser" (low level laser therapy e.g. Laserpen) or high level laser therapy must always be selected individually and depends on various factors, such as type and depth of tissue, size of the area, energy density of the laser beam, duty cycle of the modulated laser beam and as well treatment duration. The type of disease, the patient's reaction capacity and the therapy method (e.g. trigger points tolerate a strong stimulus) can also play a role.
Photoacceptor
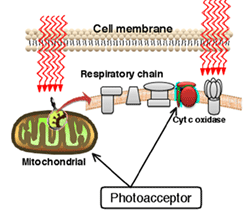
Photobiomodulation, Biostimulation, ATP-Synthesis
As already described above, laser therapy (see also Basics) unfolds one effect via the heat effect, another is the biostimulative effect, the so-called photobiomodulation and resulting cellular effects such as ATP synthesis. In addition, the photoacoustic effect also seems to be effective in modulated laser therapy (see frequency research).
The application of the laser leads to various reactions in living organisms. The laser energy is absorbed by the tissue and the cells and leads to an improvement of the cellular metabolism by also activating the respiratory control circuit.
Among other things, cytochrome c oxidase is discussed as a photoreceptor; further information on this can be found in the area of laser research (cellular effects of laser therapy, penetration depth of the laser).
The application of the laser leads to various reactions in living organisms. The laser energy is absorbed by the tissue and the cells and leads to an improvement of the cellular metabolism by also activating the respiratory control circuit.
Among other things, cytochrome c oxidase is discussed as a photoreceptor; further information on this can be found in the area of laser research (cellular effects of laser therapy, penetration depth of the laser).
How to apply the laser?
Research shows that there are three forms of application of laser therapy for biostimulation, photobiomodulation:
1. local irradiation of organs, body parts (macrosystem)
2. reflectorically via acupuncture, ear points, dermatomes (microsystem)
2. systemic, affecting the entire body (laser blood irradiation)
The decision for one or the other type of treatment depends on the orientation of the practice. A combination of the three application forms mentioned above is ideal. The therapist acts in the central area of function control via e.g. ear points and treats locally, the wound or inflammation etc. in parallel. The RJ laser devices are designed for simultaneous treatment.
1. local irradiation of organs, body parts (macrosystem)
2. reflectorically via acupuncture, ear points, dermatomes (microsystem)
2. systemic, affecting the entire body (laser blood irradiation)
The decision for one or the other type of treatment depends on the orientation of the practice. A combination of the three application forms mentioned above is ideal. The therapist acts in the central area of function control via e.g. ear points and treats locally, the wound or inflammation etc. in parallel. The RJ laser devices are designed for simultaneous treatment.




